Obesity rates among the general population are increasing, rising from 15% in 1993 to 26% in 2014.
However, for those with severe mental health problems, the rate of obesity is even higher due to the effects of medication, poor diet, alcohol misuse and less active lifestyles.
In addition, life expectancy of people living with serious mental illness is 15–20 years less than the general population and the need for parity of esteem between mental and physical health is a current priority.
As part of our role to provide advice to the NHS on specialised mental health services, PHE has published a review of evidence on obesity in adult mental health secure units and what the implications are for practice.
The impact of obesity for those in secure mental health services
Currently, around 6,000 people in the UK are detained in three high, 65 medium and 150 low secure mental health units due to their assessed risk to others or custodial sentences.
In these units, residents are not free to enter or leave at will.
A key finding of the review was that not only is obesity and overweight more prevalent in the population detained within mental health secure units (with rates of up to 80% reported) than in the general population (around 60%), patients appear to be more at risk of weight gain when detained.
Factors influencing this include a combination of medication side effects, condition-related reduction in motivation for self-care, and environmental influences.
In mental health secure units, we also found evidence that there is a high risk of weight gain following admission, stemming from the combined effects of incarceration, ease of access to high calorific food, and the potential lack of access to recommended levels of physical activity.
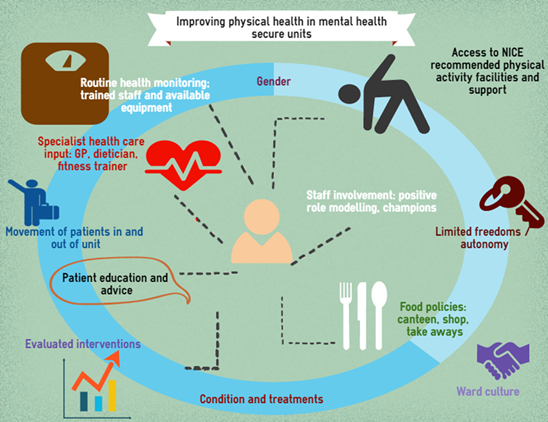
The picture above highlights some of the risk factors we identified in the literature and the interaction between them
What interventions work in tackling obesity in secure mental health units?
A small body of exploratory research identified as part of the review highlighted that in order to address obesity and achieve parity of esteem between mental and physical health in secure mental health units, a number of elements must be in place.
These include access to evidence based health promotion approaches and the associated training and equipment required, a range of dietary and physical activity strategies to reduce the obesogenic environment and changes in policy at ward level that address staff and patient behaviour change.
Interventions require attention to national guidance, such as NICE guidelines and policies, alignment with quality assessment and robust evaluation.
However, there is strong evidence of the need to tackle obesity on the ground in secure settings, for example the rates of obesity are high and can worsen over time with standard care.
Evidence suggests that small sequential steps are currently being made to change culture, policies, and staff and patient behaviours. However, there is much more to be explored in terms of tackling the problem.
Interventions need to be evaluated in larger-scale studies to assess how effective and applicable different approaches might be for specific populations, in particular those detained in secure units.
Our review conclusions recommend a focus on the following factors to reduce obesity and improve health and wellbeing:
- Implementing policies that increase access to healthier food choices and physical activities
- Encouraging staff to role model healthy behaviours
- Gradually changing ward or unit policy and culture to encourage healthy lifestyle choices
- Providing activities that are enjoyable and social.
These changes can also impact positively on feelings of confidence and wellbeing and help ease mental health problems.
A partnership approach
As well as reviewing published evidence we have engaged with service users, clinicians, commissioners and academics in the fields of mental health and obesity in the development of this review.
Our conversations highlighted that secure mental health services need guidance to assist decision making around some of the factors identified in our report, with food policies as well as access to NICE recommended levels of physical activity highlighted as key areas where support could be developed further.
While we know food policies in particular can be challenging to implement for a variety of reasons, the amount of calories that residents access over and above the daily recommendations for maintaining a healthy BMI can be detrimental to physical health in the long term.
We have identified this as an area that we will continue to explore along with our partner organisations including NHS England, the CQC, and of course service users and clinical experts going forwards.
The review has been undertaken in collaboration with PHE Yorkshire and Humber and the University of Sheffield, supported by a Medical Research Council grant.
Interested in receiving more blogs like this? Please sign up for updates via email or follow us on Twitter.

3 comments
Comment by Steven Berman (Exercise & Mental Health Professional) posted on
As a fitness professional of 30 years I can tell you that one of the key barriers to improving health and wellbeing and rates of obesity among this particular group is the lack of involvement from the fitness industry itself.
Those who choose to train as fitness instructors rarely do so with "mental health" as their primary motivation. There is little demand from fitness instructors because generally they are far more interested in working with wealthy clients and functional social groups.
I have been working with mentally unwell patients and vulnerable individuals for many years. Rarely have I come across others within the profession who also work within this arena.
However, there is also, to some extent a responsibility on the part of mental health services to acknowledge the need to incorporate physical health and wellbeing in to care plans and formal delivery strategies within both clinical and community based services.
Exercise and healthy behaviour change should always be integral to mental health services. The few of us on the fringes of the fitness industry who have a deep interest in this area of work need to be proactively courted by mental health services if we are to collectively benefit those who are currently missing out because of silo working.
Comment by Richard Sockell posted on
Richard Sockell ( technical instructor physiotherapy)
I would find it very difficult to disagree with what you have said Steven I too am a fitness professional and have worked in this "arena" for 5 years now and have witness the same barriers. It frustrates me watching the NHS try to reinvent the wheel with this, instead of looking to the fitness industry for guidance on the growing problem with obesity in mental health, and this is not just exclusive to secure wards. With a lot of the anti psychotic medication there comes many side effects ( these side effect do not out way the potential for positive results) two of these can be a slowing of the metabolism and increased appetite. After a period, one mental health issue is managed only to give another, lack of body image confidence. This can then lead to depression and social anxiety, in turn this leads to the revolving door of mental health.
Helping service users to keep fit stay fit and incorporate health life choices is a necessity. More education to front line staff on the benefits of physical activity is in my opinion the most important step. It is difficult to see a well trained experience mental health nurse struggle to explain the importance and the best way for that services user to understand, access, and maintain good health physical activity practises. This is in no way shape or form a slur on the nurses themselves but there needs to be a deeper understanding and a more robust way of getting the message of the importance of physical activity in improving mental health.
Is the fitness industry the answer.............
would be interesting to speak to you Steven
Comment by Ruth Alderson posted on
I couldn't agree with you more Steven, I too have worked in a mental health hospital as an Exercise Therapy Assistant and there needs to be more emphasis on physical activity interventions from higher up. I have chosen to go into psychiatric nursing now but I will certainly carry with me all the advice and encouragement of a fitness professional into my new role.